Module 6: Medical Complexities
Medical Conditions
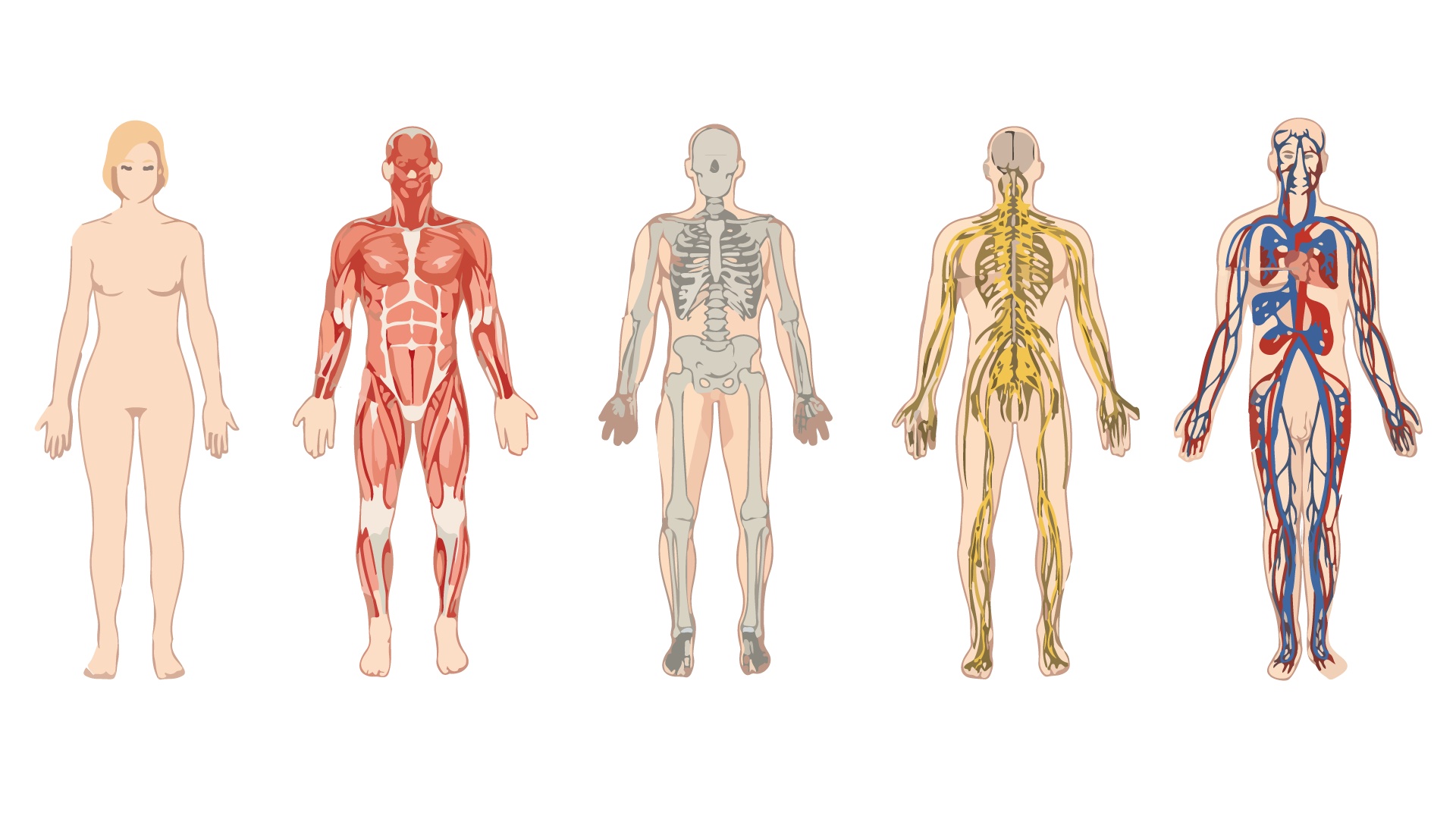
This module will introduce several of the more prevalent conditions and their impact on various body systems:
- Airway and breathing conditions
- Heart conditions
- Swallowing disorders and eating difficulties
- Gastroesophageal reflux (GERD)
- Pain
- Seizures
- Bowel and bladder function
- Orthopedic procedures
Some students have conditions such as asthma or chronic respiratory conditions that impact their airway and/or breathing. Airway and breathing interventions can include:
- Medications prescribed by a physician. Medications can be given by a school staff member who has been specifically trained by nursing support to administer the medication
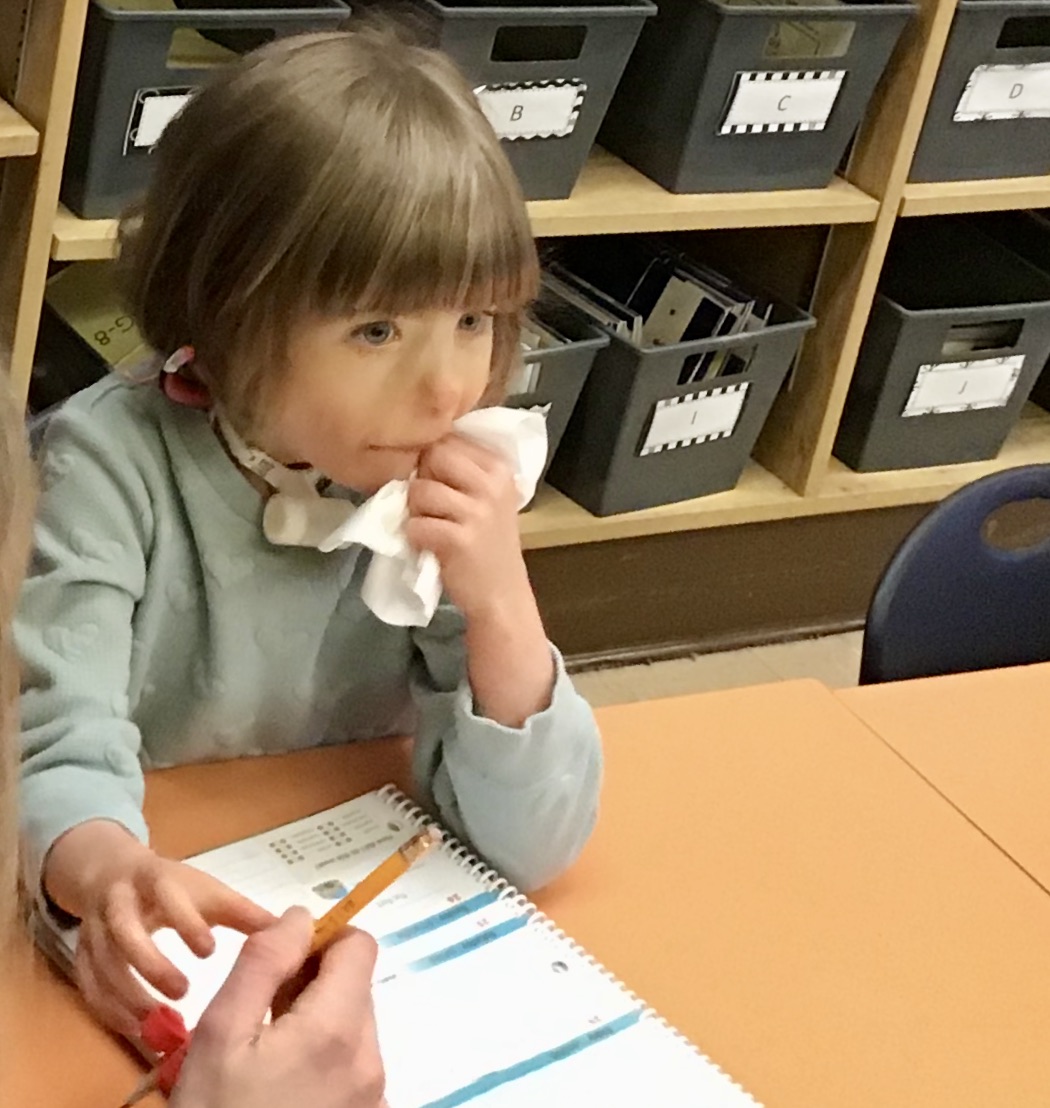
- Suctioning is a procedure that can be provided by a school staff member who has been specifically trained by nursing support to clear mucus or to assist a student to cough when they are unable to do so
- A tracheostomy assists a student to breathe with the assistance of a tube into their windpipe (trachea) that bypasses the mouth. Tracheostomy care involves keeping the area clean according to prescribed protocols. Ventilator care is provided by personnel specifically trained in these procedures. This level of care or monitoring may require a nurse to attend school with the student
The level of intervention required to ensure the student’s safety can be intrusive. Suctioning, for example, must be administered quickly when it is required and involves putting a tube into the student’s airway to clear their secretions. The procedure is often noisy and can:
- Distract classmates from classroom activities
- Disrupt the natural flow of the classroom
- Interrupt interactions with classmates
It is important to have the knowledge to explain to classmates in a reassuring way why the procedure is necessary and to answer questions they have. Having a level of comfort and understanding will assist the student with complex needs and their classmates to accept these procedures as a necessary part of what happens day to day in the classroom.
Some genetic syndromes and disorders include structural differences that affect heart function. Heart conditions primarily affect a student’s energy and endurance during activities at school. Fatigue is a common factor.
Interventions for heart conditions can include exercise restrictions and providing more time and breaks for the student to complete a task requiring movement.

Swallowing and eating can be difficult for some students and present serious safety risks during mealtimes. One of the most common safety risks is aspiration. Aspiration pneumonia is a serious infection of the lungs which can result in hospitalizations and time away from school. Risk of aspiration can be easily seen when the student gags or chokes while eating, or difficult to detect when there are no obvious signs of distress while eating. Under the direction of therapists with knowledge of swallowing disorders, interventions can be made to reduce the risk of aspiration. These interventions can include direct assistance with eating, positioning changes, altering the consistencies of food and drink, and providing additional time to eat.
A referral for a swallowing assessment will determine whether a child should be recommended for tube feeding. One consideration is that the risk of aspiration is such a safety concern that the child cannot eat food by mouth, and another consideration is when eating is so time-consuming and difficult that the child’s nutritional needs are not being met.

The most common form of tube feeding among students with complex needs is done through a gastrostomy tube, more commonly referred to as a G-tube that is placed through the abdomen directly into the stomach. The flow rate of the tube feeding formula is regulated by a pump.
It can take a long time to have a meal this way. For many students, being fed takes a significant portion of their day at school, and in these cases tube feeding is often conducted in the classroom, so the student does not miss out on valuable learning time. Specific protocols, including more time, are needed for meals and snacks.
Whether a student eats by mouth or is tube fed, specific protocols are developed, and staff members are specifically trained to safely meet the needs of each student. Students benefit from being with their classmates for the social aspect of meals and from cooking and food preparation lessons even if they are not eating in the same way.

Gastroesophageal reflux disease (GERD) is a condition whereby acid from the stomach comes up into the esophagus and mouth. It causes a painful burning sensation that can cause discomfort, pain, irritability, and can impact sleep, behaviour, and eating.
Interventions for GERD include medication and being positioned upright for a set time after eating.

Pain is well known to be a common complication of physical disability, particularly among individuals who use wheelchairs and adapted mobility (Dudgeon, Gerrard, Jensen, Rhodes, & Tyler, 2002). Pain is considered chronic when it has been present for more than six months.
Pain can be very difficult to manage. In students with complex needs, it’s often difficult to determine the location of the pain and fully understand the individual experience. Even when treated, pain and the emotional response to pain can remain. Interventions for pain include:
- Medications
- Therapies (physical, massage)
- Medical interventions (surgeries)
- Body positioning

Think about a time when you or someone you know experienced chronic pain.
- How did it impact your ability to concentrate? To do daily tasks? To interact with others?
- What were some of the emotions you experienced because of the pain?
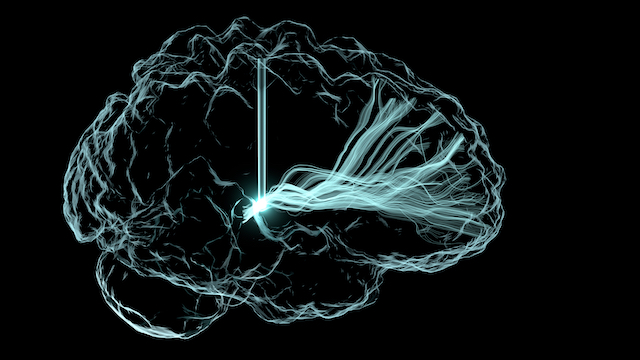
Seizures are common in students with neurological conditions. “A seizure is a burst of uncontrolled electrical activity between brain cells that causes temporary abnormalities in muscle tone or movements, behaviours, sensations or states of awareness”
John Hopkins Medicine, 2021
When most of us hear the term seizure, we think of a condition where the person’s body experiences convulsions, and the person loses consciousness. This type of seizure is now called tonic-clonic referring to the two phases of the seizure where the body stiffens (tonic) followed by the convulsive (clonic) phase.
There are many types of seizures. Seizures are differentiated by type of onset, type of impact, and level of awareness. The following table shows the differences and overlaps between onset, impact and awareness:
| Onset | Impact | Awareness | Motor Symptoms | Non-Motor Symptoms |
|---|---|---|---|---|
| Generalized Onset | Affects both sides of the brain or cells on both sides | Impaired awareness |
|
"Absence": Staring spells and brief twitching in one body part |
| Focal Onset | Origin in one area of one side of the brain | Aware and impaired awareness |
|
Changes in sensations, emotions, thinking, autonomic functions, or behaviour arrest |
| Unknown Onset | Origin is unknown, could be because the seizure is unwitnessed | Unknown level of awareness | Tonic Clonic | Behaviour arrest |
Interventions to manage seizures include medications, diet, environmental changes, and seizure support. In some cases, surgical intervention is used to eliminate or significantly reduce the frequency or intensity of the seizures:
- Medications: There are a number of medications (generally prescribed by a neurologist) that are used individually or in combination to manage seizures. Medications used to control seizures can have side effects that can affect a student’s alertness and ability to participate
- Diet: Some students with seizures not controlled with medication can benefit from a diet that is high in certain fats. This type of diet should be prescribed by a medical professional
- Environmental changes: Seizure activity can be triggered by flashing lights or excess stimulation. It is beneficial to be aware of known triggers and modify the environment or activity to limit triggering a seizure
- Seizure support: Students who have seizures need support during and after a seizure. These supports could be moving items out of the way during a seizure, providing time, rest and space post seizure, and modifying activities and learning for the remaining school day
- Surgery: Surgery could be considered for seizures that are not controlled by medication and are severely impacting quality of life. Surgery can be used to remove a focal area in the brain or to cut the connections between the two sides of the brain to prevent seizures from generalizing. Any surgical intervention will likely impact learning at least temporarily but can have long term consequences as well
The impacts of seizures vary from one individual to another. It is important to keep in mind that most seizures are not harmful but can be unsettling for the student and others. Educating students in your class about seizures will help reduce anxiety.
Every student with seizures has an individual protocol to follow when seizures occur. Familiarize yourself with the protocol and inform other staff and students about how to respond quickly and appropriately.
Students who experience seizures often need to rest and recover afterwards. They will miss out on time in the classroom and will need to be caught up on what they missed.
